Paragangliomas and Other Skull Base Tumors
Paragangliomas and Other Skull Base Tumors – About
A paraganglioma is a rare tumor that begins in certain nerve cells that are dispersed throughout the body. This tumor can affect people of any age but most often shows up between the ages of 30 and 50. The tumor is often slow growing and noncancerous (benign). But it can invade nearby parts of the body, become cancerous (malignant) and spread distantly (metastasize).
In a small percentage of head & neck paragangliomas, the abnormal cells produce hormones known as catecholamines or adrenaline, which is the fight-or-flight hormone. This may induce high blood pressure, a rapid heartbeat, flushed skin, sweating, headache and tremors.
Surgery to remove the tumor is usually the first treatment choice for a paraganglioma, if feasible. If left untreated, paragangliomata can sometimes result in severe or life-threatening damage, or progress to the point where surgical treatment is not an option. In people with cancerous and distantly spread (metastatic) paraganglioma, medicine and other treatments can help control the disease and symptoms and even extend survival.
Paragangliomas and Other Skull Base Tumors – Diagnosis
If your primary doctor thinks you may have a paraganglioma, he or she may refer you to an expert in cancer (medical oncologist), an expert in conditions of the endocrine system (endocrinologist) or a surgeon.
You may need a number of tests:
- 24-hour urine test. You may be asked to collect a urine sample every time you urinate during a 24-hour period. This will be used to assess hormone excretion into urine. You will be given written instructions on how to store, label and return the samples.
- Blood test. You may have blood drawn for laboratory testing, including an assessment of hormone levels. Talk to your doctor about special preparations, such as fasting or skipping a medication. Do not skip a dose without specific instructions from your doctor.
- Imaging tests. Your doctor may order one or more imaging tests to define as accurately as possible the location of the tumor. These studies may include an MRI, CT or specialized nuclear medicine imaging.
- Genetic testing. Paragangliomas sometimes run in families, associated with altered genes that can be transmitted from parent to child. Your doctor may have your blood tested for this. And if an altered gene is detected, your doctor may recommend that you see a genetic counselor.
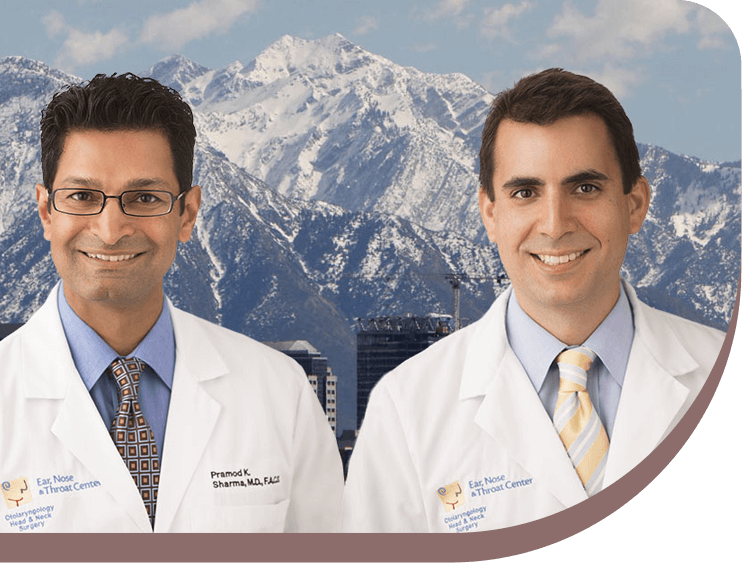
People with paragangliomas need care by an experienced, multidisciplinary team. Ask your doctor if he or she regularly treats people with this condition, as most doctors rarely (if ever) encounter paragangliomas and are unfamiliar with the best approaches to diagnosing and treating this rare tumor. Under such conditions, it is important to seek a second opinion from a team that specializes in the care of people with rare neuroendocrine tumors such as paragangliomas. Our Head & Neck Surgeons have extensive experience in managing these tumors.
Paragangliomas and Other Skull Base Tumors – Treatment
Treatment of a paraganglioma depends on where the abnormal growth is located and whether it is cancerous. A paraganglioma is considered cancerous (malignant) if it spreads to other parts of the body (metastasizes). This is a rare occurrence in paragangliomas. Cells from a cancerous (malignant) paraganglioma can migrate to lymph nodes, bone, liver, lungs or elsewhere. In people with this type of paraganglioma, it is critical to treat any elevated hormone levels and other signs and symptoms.
Treatment options include:
- Medications. Your doctor will first attempt to control symptoms caused by your paraganglioma, such as high blood pressure, if you have the type of paraganglioma that produces hormones. Drugs that usually help people with this condition include alpha blockers and beta blockers. In people with hormone-producing paragangliomas, it is critical to control blood pressure before surgery or other therapy.
- Surgery. Surgery to remove the tumor is generally the first choice for treatment, if feasible. Even if the tumor has spread, surgery is often used to reduce its size.
If paraganglioma tissue that produces hormones is disturbed, as happens during surgery, hormones in the tumor can be released and cause serious problems, such as elevated blood pressure and pulse. To prevent that, your doctor will have you prepare for surgery by taking medication to block the hormone’s effects for 7 to 14 days before surgery. You may also be asked to record your blood pressure multiple times a day, to follow a high-sodium diet and to report your blood pressure results to your medical team.
Paraganglioma surgery is done under general anesthesia. It is important that specialized surgeons and anesthesiologists be involved. You will likely need to stay in the hospital for several days after surgery. Even after successful removal of the tumor during surgery, tumors may recur. So you will need to visit your doctor regularly for follow-up appointments.
- Radiation therapy. Radiation therapy is sometimes used to help control tumor growth and improve your symptoms if other options, such as surgery, are not advisable. If the tumor is in the head or near vital nerves or blood vessels, a technique called stereotactic body radiation therapy may be used to limit damage to nearby healthy tissue.
- Thermal ablation therapy. Under some circumstances, specialized interventional radiologists may destroy tumor deposits with an approach called thermal ablation therapy.
- Clinical trials. You may be eligible for a clinical trial testing an experimental treatment.
- Watchful waiting. If the tumor is slow growing, your doctor may monitor your condition during regular follow-up appointments even if you are not undergoing therapy.

Conditions Treated
Follow us

Your Health Starts Here
"*" indicates required fields
