Our Services
Ear Conditions
We are a comprehensive diagnostic and treatment center for hearing and balance disorders, such as hearing loss, ear infections, and tinnitus.
Nose Conditions
We provide complete care of the nasal cavity, from rhinoplasty and other nasal surgeries to treatment of chronic nose bleeds, nasal obstruction, and smell disorders.
Throat Conditions
We have expert diagnosis and treatment services for issues relating to the throat, larynx, and esophagus, including chronic strep throat and tonsillitis, halitosis, and Gastroesophageal Reflux Disease (GERD).
Neurotology & Advanced Otology
Our highly skilled and trained specialists evaluate the parts of the nervous system and brain which are related to hearing and balance, and provide medical and surgical care for diseases of the ears, face, temporal bone, skull base, and related structures of the head and neck.
Advanced Head & Neck Oncology and Reconstruction
Early detection, diagnosis and treatment of head and neck cancer.
Facial Plastic Surgery
We specialize in corrective, reconstructive, and cosmetic surgeries of the nose and ears.
Sinus
Our physicians and surgeons diagnose and treat all abnormal conditions of the sinus cavities, from common sinusitis and sinus headaches to sinus fractures and tumors.
Allergies
If you are seeking relief from the discomfort of allergies, or want to find out which allergens are causing your symptoms, we offer diagnostic testing and treatment plans to help control your symptoms, prevent severe allergy attacks, and improve your quality of life.
Sleep Apnea & Snoring
We are specialists in the field of diagnosing and managing sleep apnea and snoring issues.
Thyroid & Salivary Disorders
Our board-certified physicians have specialized training in conditions affecting the thyroid and salivary glands.
Swallowing & Voice Disorders
Our team can diagnose a variety of voice disorders and medical conditions that affect the production of speech. We also treat dysphagia, which is difficulty or pain in
swallowing.
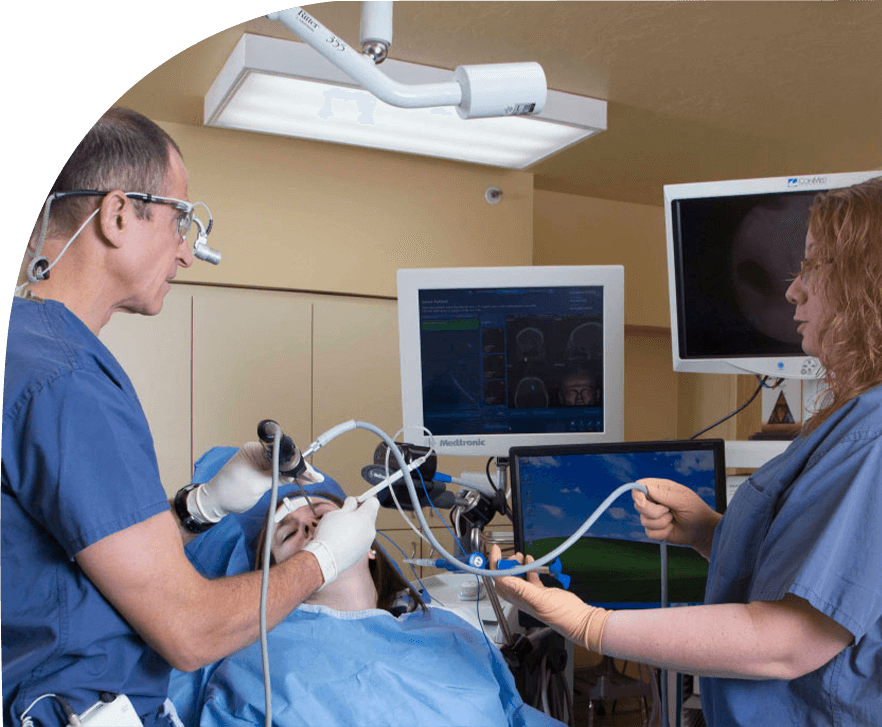
ENT Imaging
Utah’s state of the art center with a significant investment in imaging technology of the highest caliber.
Dizziness & Balance Disorders
Dizziness and balance disorders can be caused by certain health conditions, medications, or a problem in the inner ear or the brain. Vertigo,
Meniere’s Disease, and Acoustic Neuroma are common balance disorders that are diagnosed and treated by our expert physicians.
Hearing & Hearing Aids
We offer a complete range of audiology services to help treat hearing loss and improve your quality of life.
Surgical Center
We have the only outpatient center exclusively devoted to the treatment of ear, nose, and throat conditions.
Oculofacial Plastic Surgery
Esthetic and reconstructive surgery of the eyelids and face.
Our Physicians
Ear, Nose and Throat Center physicians deliver excellence in compassionate, comprehensive care. ENT Center physicians in Salt Lake City, Draper, Riverton, Millcreek, Heber and Park City Utah are certified by the American Board of Otolaryngology-Head and Neck Surgery. Expertise is a given.
Just as important, we bring our passion for medicine and friendly approach to every exam or consultation. We will listen and respond to your needs, with recommendations and treatment that will help maintain and enhance your health. We work hard to deliver exceptional care for our patients across Utah’s Wasatch Front.
Follow us

Your Health Starts Here
"*" indicates required fields